Understanding Antigens in the Immune System and Biotechnology
What is an Antigen?
An antigen is any substance that can trigger an immune response in the body. Antigens are typically proteins or polysaccharides that are recognized as foreign or potentially harmful by the immune system. When an antigen enters the body, it stimulates the production of antibodies or the activation of specific immune cells to neutralize or eliminate the perceived threat.
Types of Antigens
Antigens can be classified into different types based on their origin and characteristics:
Exogenous Antigens
Exogenous antigens are foreign substances that enter the body from the external environment. Examples include bacteria, viruses, fungi, and other pathogens. These antigens are typically recognized by the immune system as non-self and trigger an immune response to eliminate the invading organism.
Endogenous Antigens
Endogenous antigens are substances that originate within the body's own cells. These antigens can be derived from normal cellular proteins or from abnormal proteins produced by cancer cells or virus-infected cells. In some cases, the immune system may mistakenly recognize self-antigens as foreign, leading to autoimmune disorders.
Tumor-Associated Antigens
Tumor-associated antigens (TAAs) are proteins expressed by cancer cells that can elicit an immune response. TAAs can be overexpressed normal proteins, mutated proteins, or proteins that are normally expressed only during fetal development. Identifying and targeting TAAs is a key strategy in cancer immunotherapy.
Antigen Presentation
For the immune system to recognize and respond to an antigen, the antigen must be presented to immune cells in a specific way. This process is known as antigen presentation and involves specialized cells called antigen-presenting cells (APCs).
Major Histocompatibility Complex (MHC)
Antigen presentation occurs through the major histocompatibility complex (MHC) molecules on the surface of APCs. MHC molecules bind to peptide fragments derived from the antigen and display them on the cell surface for recognition by T lymphocytes. There are two main classes of MHC molecules:
- MHC class I molecules present peptides from intracellular antigens to CD8+ T cells, which are involved in the elimination of virus-infected cells and cancer cells.
- MHC class II molecules present peptides from extracellular antigens to CD4+ T cells, which activate other immune cells and orchestrate the immune response.
Antigen Processing
Before an antigen can be presented by MHC molecules, it must undergo a process called antigen processing. Antigen processing involves the degradation of the antigen into smaller peptide fragments that can be loaded onto MHC molecules. This process occurs in different cellular compartments depending on the type of antigen:
- Intracellular antigens, such as viral proteins, are processed in the cytosol and presented by MHC class I molecules.
- Extracellular antigens, such as bacterial proteins, are internalized by APCs, processed in endosomes or lysosomes, and presented by MHC class II molecules.
Antibody-Antigen Interactions
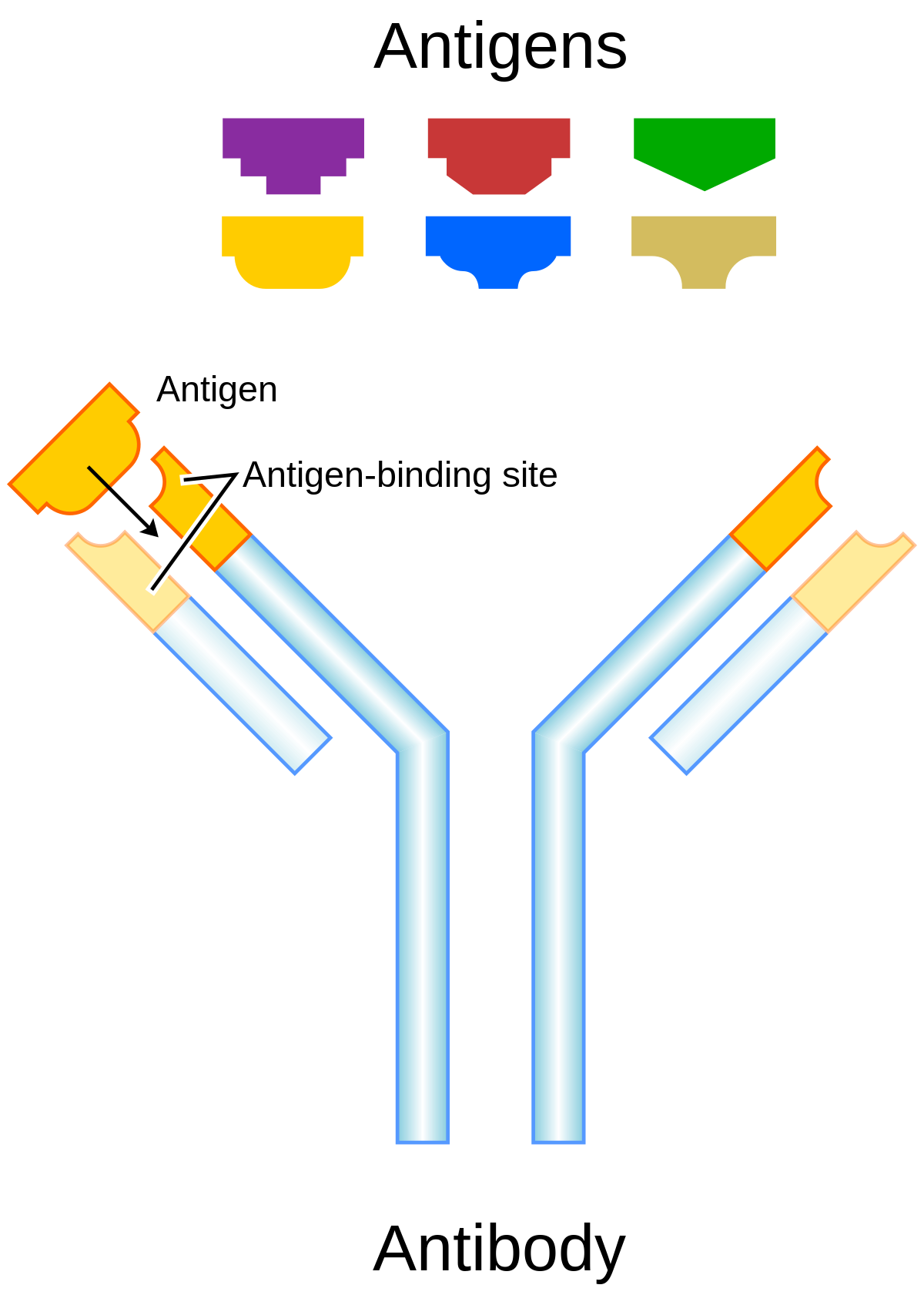
The specific recognition and binding of antigens by antibodies is a fundamental aspect of the immune response. Antibodies, also known as immunoglobulins, are Y-shaped proteins produced by B lymphocytes that can bind to specific epitopes on an antigen.
Epitopes
An epitope, also known as an antigenic determinant, is the specific region of an antigen that is recognized and bound by an antibody or T cell receptor. Epitopes are typically short sequences of amino acids or sugars that are exposed on the surface of the antigen. The specificity of the immune response is determined by the unique epitopes recognized by individual antibodies and T cell receptors.
Affinity and Avidity
The strength of the antibody-antigen interaction is determined by two key factors: affinity and avidity.
- Affinity refers to the strength of the binding between a single antibody binding site (paratope) and a single epitope on the antigen. Higher affinity interactions result in stronger and more stable binding.
- Avidity refers to the overall strength of the interaction between multiple antibody binding sites and multiple epitopes on the antigen. Avidity takes into account the cumulative effect of multiple low-affinity interactions, resulting in a stronger overall binding.
Antigens in Allergy and Hypersensitivity Reactions
Antigens can also be involved in the development of allergies and hypersensitivity reactions. In these cases, the immune system mounts an excessive or inappropriate response to an otherwise harmless antigen, leading to symptoms such as itching, swelling, and difficulty breathing.
Allergens
Allergens are antigens that trigger an allergic response in susceptible individuals. Common allergens include proteins found in pollen, pet dander, dust mites, and certain foods. In allergic individuals, exposure to these antigens leads to the production of IgE antibodies, which bind to mast cells and basophils. Subsequent exposure to the allergen causes cross-linking of the IgE antibodies, triggering the release of histamine and other inflammatory mediators that cause the symptoms of an allergic reaction.
Hypersensitivity Reactions
Hypersensitivity reactions are exaggerated or inappropriate immune responses to antigens. There are four main types of hypersensitivity reactions:
- Type I (immediate) hypersensitivity: Mediated by IgE antibodies and involves the release of histamine and other inflammatory mediators, as seen in allergic reactions.
- Type II (cytotoxic) hypersensitivity: Involves the binding of IgG or IgM antibodies to cell surface antigens, leading to cell destruction by complement activation or antibody-dependent cell-mediated cytotoxicity.
- Type III (immune complex) hypersensitivity: Occurs when antigen-antibody complexes deposit in tissues, causing inflammation and damage.
- Type IV (delayed) hypersensitivity: Mediated by T cells and involves the release of cytokines that attract and activate macrophages, leading to tissue damage.
Antigen Diversity and Antigenic Variation
Antigen diversity and antigenic variation are important concepts in understanding the complexity of the immune response and the challenges in developing effective vaccines and treatments against certain pathogens.
Antigen Diversity
Antigen diversity refers to the wide range of different antigens that the immune system can recognize and respond to. This diversity is essential for the immune system to provide broad protection against various pathogens and foreign substances. The incredible diversity of antigens is made possible by the genetic recombination and somatic hypermutation processes that occur during the development of B and T lymphocytes, allowing for the generation of a vast repertoire of antigen-specific receptors.
Antigenic Variation
Antigenic variation is a mechanism employed by some pathogens to evade the immune response by altering their surface antigens over time. This process involves the expression of different antigenic variants within a pathogen population, making it difficult for the immune system to recognize and eliminate the pathogen effectively. Examples of pathogens that employ antigenic variation include:
- Influenza viruses: These viruses undergo antigenic drift (minor changes in surface antigens) and antigenic shift (major changes due to genetic reassortment), necessitating the development of new flu vaccines each year.
- HIV: The high mutation rate of HIV leads to the rapid generation of antigenic variants, contributing to the difficulty in developing an effective HIV vaccine.
- Trypanosoma brucei: This parasitic protozoan, which causes African sleeping sickness, periodically switches its variant surface glycoprotein (VSG) coat, allowing it to evade the host's immune response.
Understanding antigen diversity and antigenic variation is crucial for developing strategies to combat infectious diseases and design more effective vaccines and immunotherapies.
Applications of Antigens in Biotechnology
Understanding and harnessing the properties of antigens has led to numerous applications in biotechnology and medicine:
Vaccines
Vaccines are one of the most important applications of antigens in biotechnology. Vaccines contain attenuated or inactivated pathogens, or specific antigenic components of pathogens, that stimulate the immune system to develop protective immunity against future infections. By exposing the immune system to a controlled dose of the antigen, vaccines can induce the production of specific antibodies and the formation of memory B and T cells, providing long-lasting protection.
Monoclonal Antibodies
Monoclonal antibodies (mAbs) are highly specific antibodies produced by a single clone of B cells. mAbs are generated by fusing B cells from an immunized animal with immortal myeloma cells, creating hybrid cells called hybridomas that can secrete large quantities of a specific antibody. mAbs have numerous applications in research, diagnostics, and therapeutics, including targeted drug delivery, cancer immunotherapy, and the treatment of autoimmune diseases.
Diagnostic Assays
Antigens are widely used in diagnostic assays to detect the presence of specific pathogens, biomarkers, or antibodies in patient samples. Examples include enzyme-linked immunosorbent assays (ELISA), lateral flow assays (e.g., pregnancy tests), and immunohistochemistry. These assays rely on the specific recognition of antigens by antibodies to generate a detectable signal, allowing for the rapid and sensitive diagnosis of various diseases and conditions.
Challenges and Future Perspectives
Despite the significant advances in our understanding of antigens and their applications in biotechnology, several challenges remain. One of the main challenges is the development of effective vaccines and immunotherapies against complex pathogens and diseases, such as HIV, malaria, and cancer. These pathogens often employ sophisticated mechanisms to evade or suppress the immune response, making it difficult to identify and target the relevant antigens.
Future research in antigen-related biotechnology will focus on the development of novel strategies to overcome these challenges. This may involve the identification of new antigenic targets, the design of more potent and specific antibodies, and the optimization of vaccine and immunotherapy formulations. Additionally, the integration of cutting-edge technologies, such as single-cell sequencing, structural biology, and computational modeling, will provide new insights into the molecular basis of antigen recognition and inform the rational design of improved immunological interventions.
Further Reading
Nature Reviews Immunology, A guide to antigen processing and presentation
Microbiological Research, Diagnostic accuracy of rapid antigen test for SARS-CoV-2
Nature Reviews Clinical Oncology, Antigen presentation in cancer — mechanisms and clinical implications for immunotherapy
